Sharon Kimbrough went to the Black Women’s Expo in Atlanta to sell her memoir. Getting tested for Alzheimer’s was the furthest thing on her mind, but when nurses from Eli Lilly approached her about the company’s new trial, she decided to let them draw her blood.
“I had two family members that had Alzheimer’s,” said Kimbrough, a retired advertising executive. “Sometimes I have memory issues and some of it in older age happens. But it could be something else.”
Eli Lilly drove two mobile labs to the Black women’s gathering, to recruit older Black women for a new trial. The drug maker developed the labs on wheels in 2020, to keep its clinical trials going in the first year of the Covid pandemic.
“We had to get really creative about how we were able to have outreach in the community,” explained Lashan Neville, Eli Lilly senior director for central clinical services.
What began out of necessity, has now become a vehicle for driving diversity in the drug maker’s trials, and building trust in communities of color which have traditionally been under-represented in clinical research.
Tuskegee legacy
Black patients have generally shown more hesitancy to participate in clinical trials than whites. A study by the Alzheimer’s Association found that 62% of African Americans think clinical research is biased against people of color.
Part of the mistrust may stem from the legacy of the 20th century Tuskegee syphilis experiment, in which government researchers withheld treatment from Black participants, but not their white counterparts, in order to study the progression of the disease.
Eli Lilly researchers say leveraging the mobile research units to meet patients at community events has helped recruit more diverse trial participants, especially in the Black community.
“We’re educating people about clinical research … how to be a part of it, how they can use research, as a way, a different way for them to get access to health care,” Neville said.
Decentralized trials
Finding and enrolling patients can be among the most costly and time-consuming part of clinical trials. The National Bureau of Economic Research estimates the median price at $19 million. Traditionally, clinical trials have centered around academic medical centers, but the facilities are often too far to travel for patients not living in large metropolitan areas.
Retailers CVS Health, Walgreens and Kroger have announced new initiatives to provide clinical trial enrollment and follow-up services in their pharmacy clinics, which could help researchers reach patients in their communities, closer to home.
Increasingly, drug makers are taking a more direct route to patient outreach to speed up the enrollment process through social media.
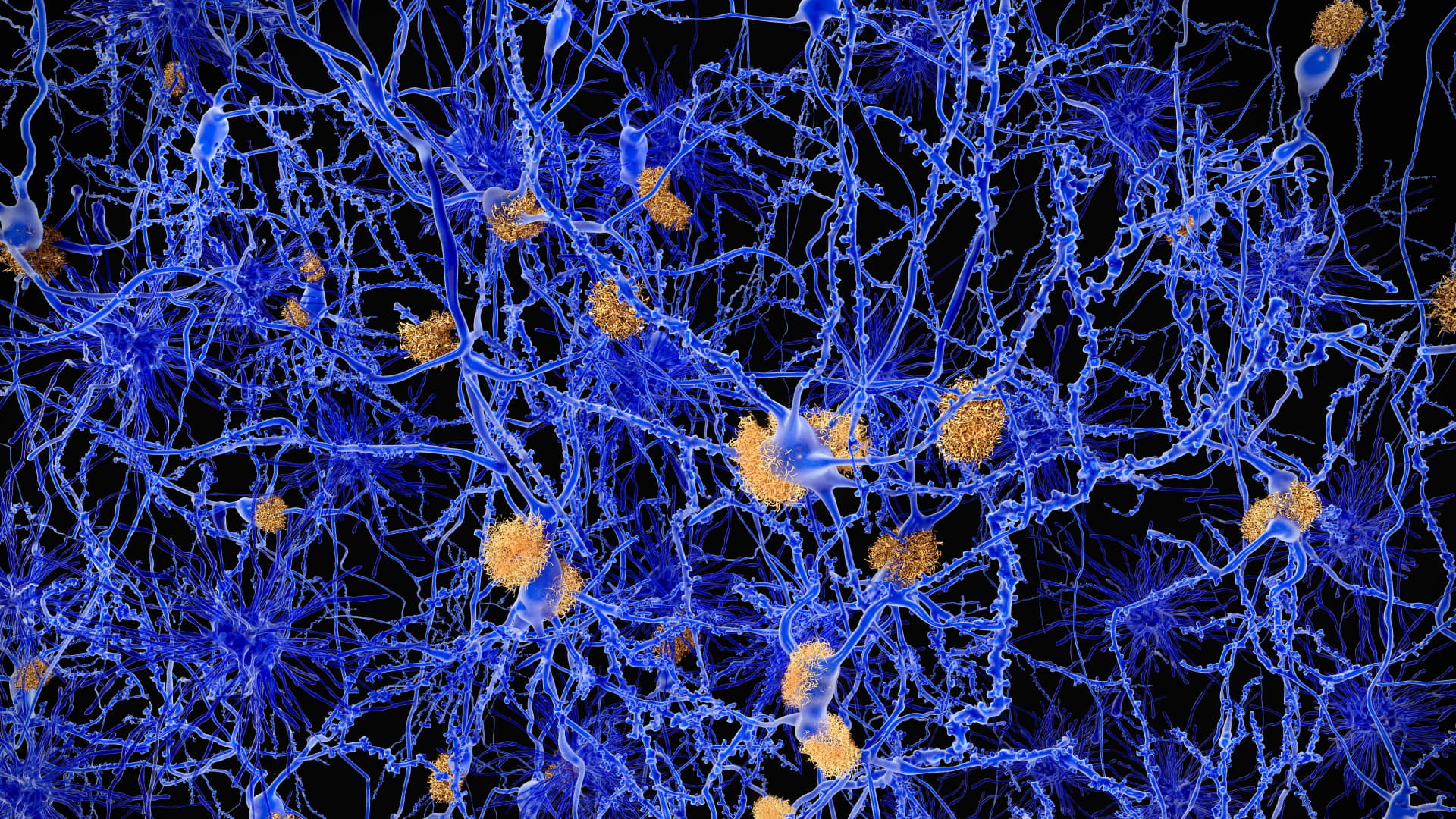
Amyloid plaques accumulate outside neurons. Amyloid plaques are characteristic features of Alzheimer’s disease. They lead to a degeneration of the affected neurons.
Getty Images
Pre-pandemic, the top three ways most patients learned about trials were through traditional advertising, their doctors and research centers according to a survey by the Center for Information & Study on Clinical Research. Social media didn’t even rank in the top ten. By 2021, while advertising remained the top source, social media replaced doctors as the second most-likely way trial participants learned about clinical studies.
Pfizer CEO Albert Bourla says social media has become a useful way to recruit participants.
“We go with social media in addition to all the other measures that we take, to targeting populations that … are underrepresented in clinical trials,” Bourla told CNBC. “We do that because not only will that increase the representation of them but also we are increasing, in general, the speed with which we can recruit patients in the study.”
FDA push for diversity
The Food and Drug Administration has encouraged drug makers to broaden criteria for enrolling trial participants to increase diversity in general, to encompass racial, geographic and age differences. Blacks are 1.5 to 2 times as likely as whites to develop Alzheimer’s Disease. Yet, one academic review of pre-pandemic dementia research found just 4% of participants in trials that reported race and ethnicity were Black or Hispanic.
FDA commissioner Dr. Robert Califf applauds efforts to decentralize trial sites, and using technology and mobile labs to make trials more accessible to a more diverse swath of Americans. Though, he says, there are limits.
“In some cases, it’s not the right thing to do. If you’re studying, for example, a new drug that hasn’t been tested in many people, you may need to be in a very intense environment and an academic medical center,” Dr. Califf told CNBC. “For other kinds of trials, it’s absolutely the right thing to do.”
Sharon Kimbrough is willing to do her part to help boost representation, but she’s hoping she won’t qualify for the Lilly trial. The blood sample she gave in the mobile lab is being analyzed for elevated Tau protein levels, which has been associated with Alzheimer’s Disease.
“I hope I find out I don’t have the protein that means I likely have Alzheimer’s,” she said, adding “that would be the joy of it all.”
She’s still awaiting the blood test outcome, but in her memoir, Kimbrough writes about faith helping her overcome life’s personal struggles. A positive result would usher in a whole new chapter.