A measles outbreak in Central Ohio has surpassed 80 cases, concentrated among unvaccinated children. According to available data Tuesday from the city of Columbus, 74 of the cases were in unvaccinated children, four were in partially vaccinated children who haven’t yet received their second dose and another four were in children whose vaccine status was unknown.
Twenty-three of the cases have been in children under 1 year old, which is too young for them to be eligible for the vaccine.
In late November, the US Centers for Disease Control and Prevention and the World Health Organization warned over a huge disruption in child measles vaccinations. Nearly 40 million children worldwide missed their measles vaccine in 2021, the health agencies said.
At face value, under 100 reported cases doesn’t seem like a big deal, especially as we grapple with other diseases, including COVID-19, the flu and RSV. But to Dr. Steven Abelowitz, medical director of Coastal Kids pediatric medical group, the current growth of measles and the undervaccination of children worldwide is “more than a canary in the coal mine.”
In 2019, right before the pandemic, the US saw the most reported measles cases since the 1990s. The majority of cases were in underimmunized communities, and 89% of people with measles were unvaccinated or had an unknown vaccine status.
“Ironically, the silver lining of COVID was we had 13 cases,” Abelowitz said, referring to the CDC’s official count of measles cases in 2020. “Now that we’re starting to see this outbreak here, this is what we were very fearful of.”
Measles has been considered eliminated from the US since 2000, which means that while there have been isolated outbreaks, there hasn’t been “continuous transmission of the disease for more than 12 months.” In the decade before 1963, when the measles vaccine became available, 3 million to 4 million people were infected and 48,000 were hospitalized per year.
There’s a smattering of measles cases each year in the US, with small outbreaks sometimes occurring in communities with lower than normal vaccination rates. And while vaccinated children and adults have little to fear when it comes to measles, lapses in vaccine uptake and concentrated outbreaks once again call attention to what happens when infectious diseases find an opportunity to spread.
Ross Kedl, professor of immunology and microbiology at the University of Colorado Anschutz Medical Campus, said that it’s “not a coincidence” that the Ohio measles outbreak is concentrated among unvaccinated children.
“If it finds itself in a susceptible population and the right circumstances — which the holidays present quite nicely — it can grow pretty quickly,” Kedl said.
Here’s what to know.
What is measles and what are the symptoms?
Measles is a highly contagious, airborne disease that causes fever, a red rash, a cough and red eyes. It’s so contagious that as many as 9 in 10 people who don’t have protection (either through vaccination or prior infection) will get it, according to the CDC.
Symptoms typically appear between seven and 14 days after an exposure, and the rash will follow three to five days after the first symptoms, according to the CDC.
Many people are at risk for complications from measles, including young children under age 5, adults over age 20, those who are pregnant and people with compromised immune systems.
Abelowitz says that severity-wise, measles is “significantly higher than most viruses we’re exposed to.”
According to the CDC, about one in five people who are unvaccinated and get measles will be hospitalized.
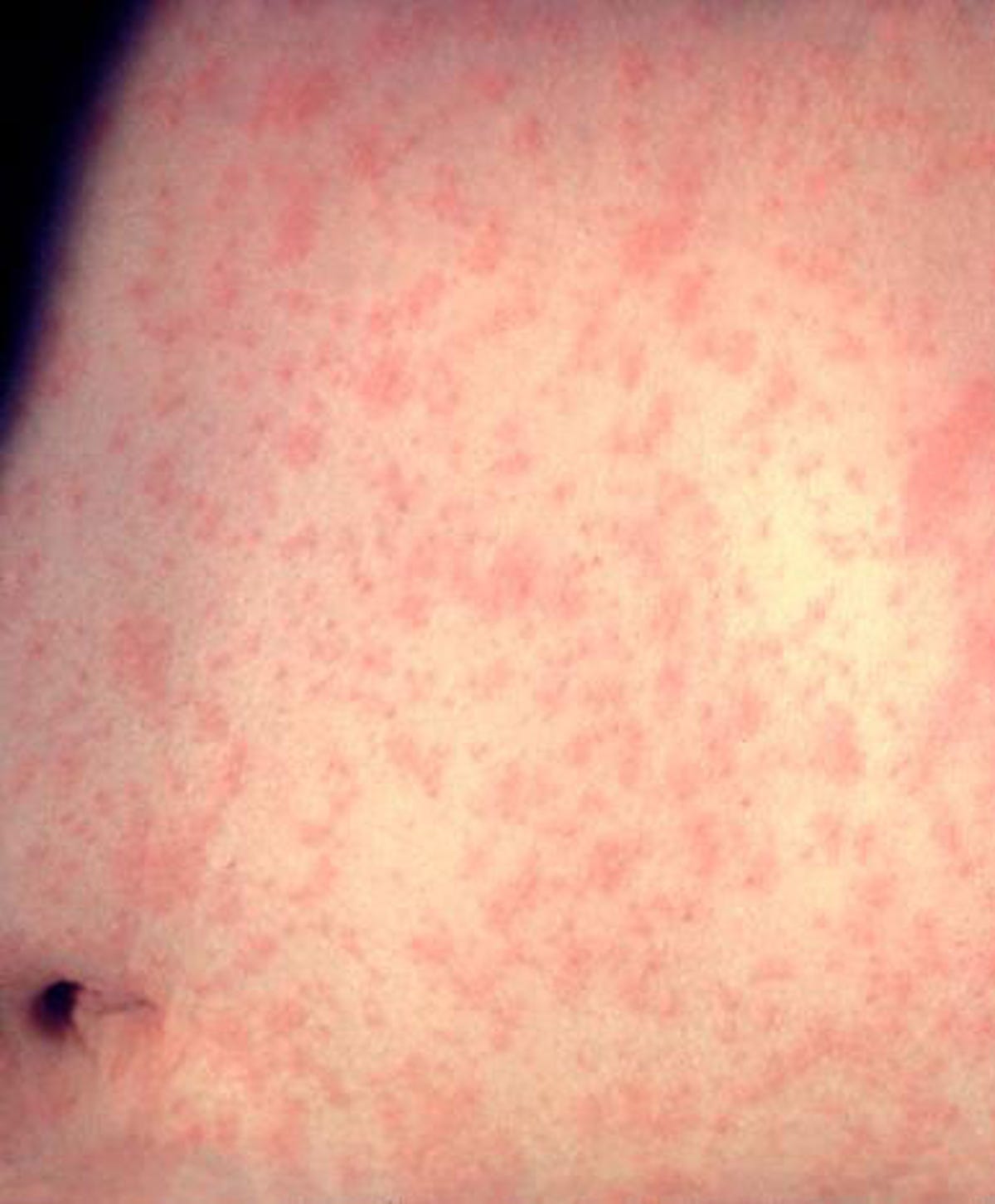
An example of measles after three days with the rash.
US Centers for Disease Control and Prevention
About the measles vaccine
Vaccination against measles is either covered by the MMR vaccine or the MMRV vaccine. Both protect against multiple diseases including measles, mumps and rubella, but MMRV includes varicella too, which is the virus that causes chickenpox. For a complete comparison between the vaccines, check out this chart from the CDC.
The American Academy of Pediatrics and the CDC recommend that all children get two doses of the measles vaccine: one shot at 12 to 15 months, and another one at 4 to 6 years.
Most people in the US have been vaccinated against measles. This protection is considered lifelong: one dose is about 93% effective, and two doses are about 97% effective, with a range of 67% to 100%, per the CDC. If you weren’t, or you’re unsure of your vaccination record, reach out to your doctor. You may get another MMR vaccine dose if you don’t have documentation, according to the CDC.
And if you were born before 1957 — regardless of your vaccination status — you also have measles protection in the CDC’s eyes, because you probably had it as a child.
What you can do about it
Vaccinated adults have very little to worry about, measles-wise. If you’re in the Columbus area, Ohio’s Department of Health has more information about sites where people could’ve been exposed and what to do.
But if you’re the parent of a young child who missed one or both doses of the measles vaccine, reach out to your pediatrician as soon as you can. Getting deeper into the holiday season where even more people will be traveling, it’s extra important to make that phone call, according to Abelowitz.
This applies not only to children in the US, but to people living in all countries.
“For three years, we have been sounding the alarm about the declining rates of vaccination and the increasing risk to children’s health globally,” Ephrem Tekle Lemango, UNICEF’s chief of immunization, said in a news release last month. “We have a short window of opportunity to urgently make up for lost ground in measles vaccination and protect every child. The time for decisive action is now.”
According to Kedl, the Columbus outbreak is “consistent with the next step of things” when measles vaccination rates continue to wane, adding that “the next thing that will likely happen is you’ll see an increased frequency of outbreak.”
“This is not a problem that needs a solution,” Kedl said. “This is a solution in need of acceptance.”
The information contained in this article is for educational and informational purposes only and is not intended as health or medical advice. Always consult a physician or other qualified health provider regarding any questions you may have about a medical condition or health objectives.
